Top image: Pavel Danilyuk / Pexels
It’s my lunch hour. But instead of sweating it out in a queue at Maxwell Food Centre with the rest of the CBD crowd, I’m standing in a tiny, freezing room with three sexually transmitted disease (STD) swab kits laid before me.
I’m at a private clinic that promises “quick, confidential, and fuss-free” STD, or sexually transmitted infection (STI), screenings. It’s located just 10 minutes from the office, but I specifically made the appointment on a day I didn’t have to be in the office. STD testing isn’t part of most colleagues’ water cooler conversations, and I didn’t want to have to explain where I was rushing off to.
(Ironically, here I am writing about the topic for all to read.)
I’m not here alone, though. As I wash my hands in preparation to swab myself, my partner’s outside scrolling through his phone. Soon, it’ll be his turn. Not to stuff a cotton swab up his vagina, no. He simply needs to pee in a cup. I’m jealous.

Sexually Active? You Should Probably Get an STD Test
We’re here for a simple reason. We started talking about having unprotected sex about a month into the relationship. Since we both have had other sexual partners, I brought up STD testing. It only made sense to get a clean bill of health before we did the dirty.
It could very well have been an awkward conversation, but he was incredibly open and even suggested we “make it a date”. Modern romance, everyone.
We’d both come out of long-term relationships and hadn’t gotten tested before. It took a good few days of research before we chose a clinic and booked our appointments.
It was only when I started Googling STD testing in Singapore, however, that I realised how little I (and probably many other Singaporeans) knew.
But we’re on the right track, according to Dr Tan Kok Kuan of Dr Tan Medical Centre, a private clinic that offers STD and human immunodeficiency virus (HIV) screenings. Dr Tan tells me all sexually active people should be getting tested regularly. ‘Regularly’ means at least once a year.
“I know you are expecting me to say [everyone should get tested] except for people in mutually monogamous relationships. But, as much as I want to have faith in the human race, I think people should just screen to protect themselves.”
Fair point. Being blindsided by infidelity is bad enough. I can’t imagine adding an STD on top of that.
Even those who have been in monogamous relationships should get tested before moving on to a new partner, says Dr Tan.
“This is to prevent them from unknowingly bringing any infections into the relationship. This is not only for each other’s physical well-being but also to prevent any misunderstandings later on. Given that many STIs can be symptom-free, people may unknowingly be infecting their partners.”
Down the STD Testing Rabbit Hole We Go
This is news to me. Like many in my generation (I’m 28, if you must know), sex education and information on STDs were limited to what I learnt in school. And my conservative mother would have sooner dropped dead than explain the birds and the bees to me.
Most of us have a vague idea of how STDs work, but that isn’t good enough, especially if you’re sexually active. Sex education in school mainly promotes abstinence before marriage and doesn’t really cater much to sexually active young adults (at least in my personal opinion). STDs are covered, but the focus is on how they’re spread and treated.
I was never taught the importance of regular testing. Nor was I taught about things like incubation or window periods.
Different types of HIV tests have different window periods. A rapid antigen test can detect HIV 18 to 90 days after exposure. A nucleic acid test can detect HIV 10 to 33 days after exposure.
When my partner and I first decided to get tested together and went down the Google rabbit hole, the information we found was nothing short of overwhelming. There are different types of clinics in Singapore, each with various pros and cons.
There are private clinics, which are unsurprisingly more expensive. There’s also the DSC clinic (part of National Skin Centre) which offers subsidised testing. The catch, however, is that testing at DSC clinic is not anonymous. This means that the clinic is legally obligated to inform the Ministry of Health (MOH) of a positive HIV diagnosis.
A colleague who recently visited DSC for STI testing tells me that this was why he’d skipped out on getting an HIV test during his appointment.
Liam*, who is in his early 20s, is here on a student pass. He tells me that anonymous testing at another clinic is probably the safer choice for him since he doesn’t have to worry about the Ministry of Education (MOE) finding out in the unlikely event of a positive HIV test.
Another thing that caught my partner and me off guard was the cost of testing. DSC Clinic charges lower prices (think $10.90 for HIV tests and $13 for syphilis tests), but it can take weeks or months to secure an appointment.
I know this because I tried to make an appointment but was assigned a slot over a month later.
We eventually went for the fastest and most convenient option, which was express testing at a private clinic. We secured appointments within a week and would receive our results via email within three to five working days.
But it came at a cost. A comprehensive test (HIV, chlamydia, gonorrhoea, mycoplasma hominis, ureaplasma, trichomonas, and candida, among others) cost us close to $400 each. Each!

It’s a Date
I gotta say, I highly recommend making a date out of STD testing—it made things just a little less daunting. The promise of brunch after our joint medical appointments helped.
Despite our preliminary research, we were both still slightly clueless when we turned up at the clinic.
The place appeared to be designed for maximum privacy. A frosted glass door blocked the reception area from prying eyes and slid open to reveal two friendly clinic staff.
We were asked to decide which tests we wanted. We chose all the tests we could get, just to be safe.
Everything was fuss-free (we were in and out of there within 40 minutes) but there were some hiccups. For one, we learned that we had to abstain from food and drinks for our HIV rapid test, which was done by swabbing the inside of the mouth. I’d stupidly showed up to the clinic sipping on an iced coffee. In the end, I had to rinse my mouth and wait 30 minutes to get swabbed.
For me, the test consisted of three vaginal swabs. For my partner, it was a urine test.
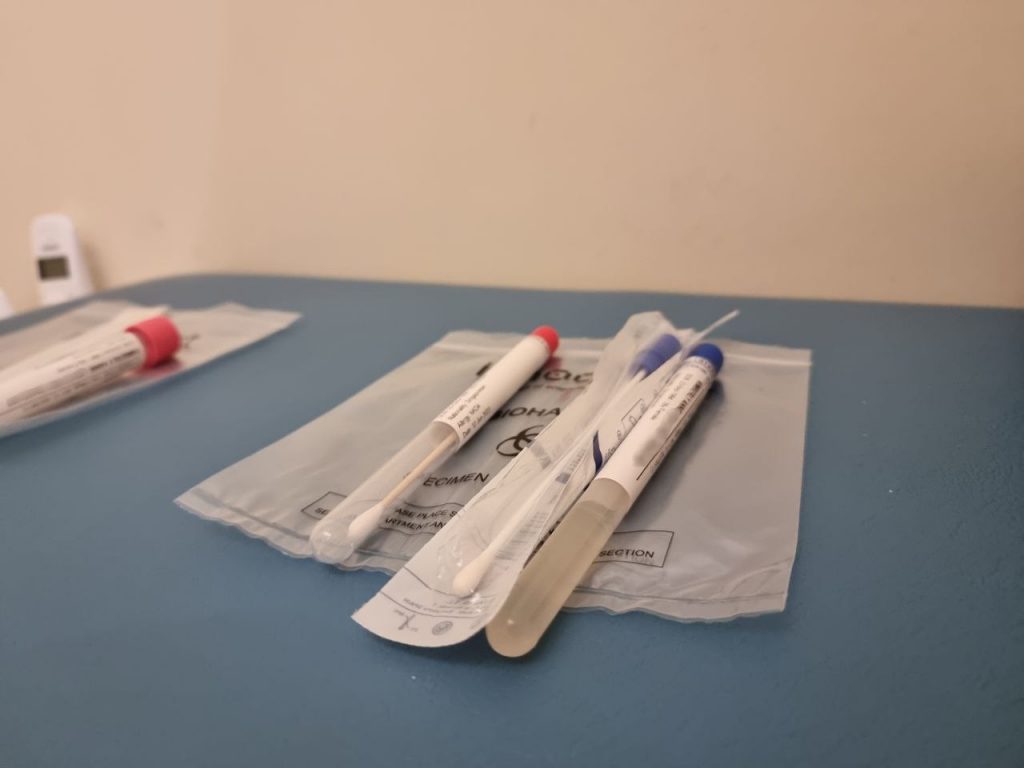
The staff shoved the swabs in my hand and gave me some very brief instructions on how to handle the samples to avoid any contamination. All I could think about while she briefed me was how similar the swabs looked to the ones used for Covid-19 rapid tests.
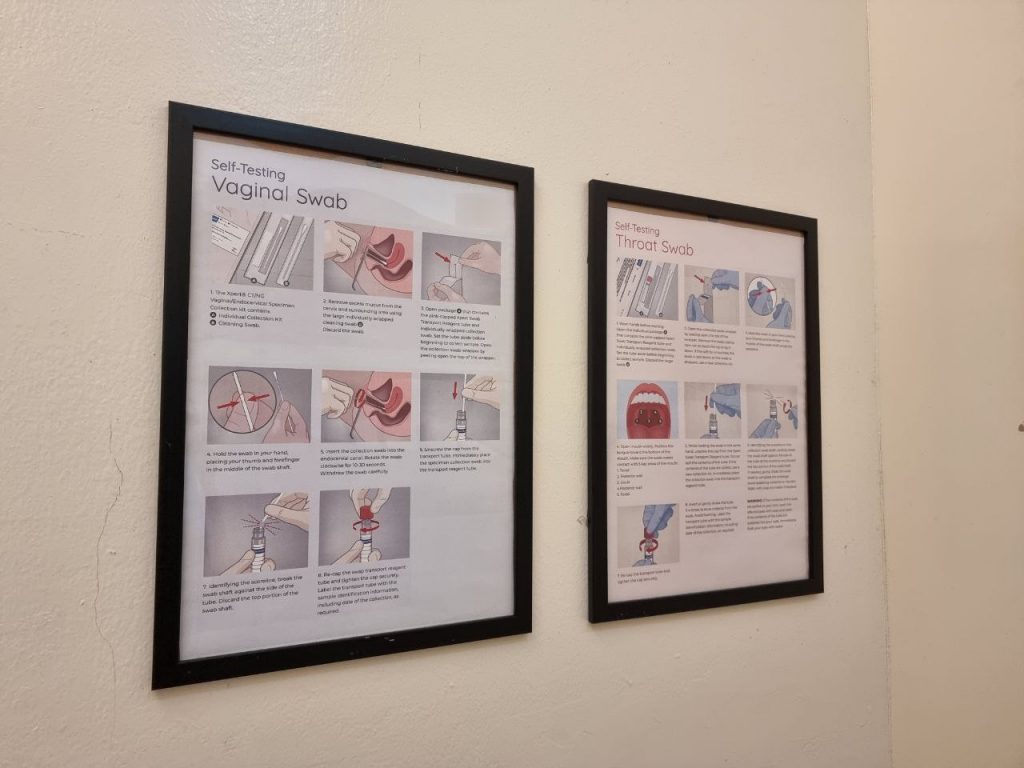
Then it was time for the main event: The swabbing. I was left in a private room to do the swabbing myself. This might be a draw for those who are a little more skittish about having another person perform the procedure. But I kinda wished I could have just whipped off my jeans, laid back and let a professional do their thing.
Really, I was just terrified I’d do it wrongly. Sure, sticking a cotton swab up your vagina is pretty straightforward, but a barrage of questions swirled in my mind. How deep did I have to go? Did I have to clean the area beforehand?
The confusion only intensified when I read the infographics on the wall (one poster contained instructions for a rectal swab). I ended up having to leave the room and clarify with the staff where exactly I was meant to be sticking the cotton swabs.
It turned out that all three swabs were supposed to be vaginal. Silly me.
Questions We Should Have Asked
Things were smooth sailing after that, thank god. I’ll spare you the details, but it really is just like a Covid test: Stick it up an orifice, swirl it around a few times, and carefully seal it up in a container.
As for my partner, things were a lot more straightforward. His was a simple urine test done at the nearby toilet. The only issue he really had was the awkwardness of walking past the lunch crowds while holding his jar of urine.
“I kind of tried to hide it,” he says.
I’ve obviously only been to one clinic, but from what Dr Tan tells me, the experience can vary among different clinics.
We weren’t made to undergo a pre-testing consult with a doctor. But Dr Tan shares that it’s an important part of the process: “Doctors still have to explain to the patient carefully the implications of testing, what tests are required, what tests are not required or cannot be done (and why). So that the patient can then plan their lifestyle within the limitations of testing.”
Perhaps a pre-test consult could have saved me a good chunk of the $400 I’d shelled out. Dr Tan says that there is no one definition of a “full test”. A “full test” at one clinic may very well differ from that offered at another clinic.
“Personally, I think there is a lot of excessive testing leading to very high medical bills. Understandably, patients want an absolute guarantee that they do not have any STDs. This, unfortunately, is not possible. There are diseases we can screen for and diseases we cannot screen for.”
Dr Tan raises the example of human papillomavirus (HPV), a group of viruses, some of which can cause genital warts or cancer.
It’s possible to screen for cancer-causing HPV in women but not in men, he says. It’s also not possible to screen for the strain of HPV that causes genital warts in both men and women.
That’s not to say you shouldn’t still get screened. It’s just not realistic to screen for every single STD in existence.
Another pertinent point that should be brought up before any STD testing is which sites to test, Dr Tan tells me.
“Most doctors will do a blood test, a urine test and perhaps a vaginal swab for women. Few would talk to their patients about swabbing the throat or even the anus. So this potentially leaves areas that have not been screened.”
This was news to me—the clinic I’d gone to didn’t bring this up. Knowing what I know now, I’d probably have gone with a clinic that required a doctor’s consultation before testing. An expensive lesson, I suppose.

STD Testing: Not the Most Romantic Topic
It would honestly have been quite nerve-wracking if I’d gotten the test done alone. But it’s definitely not an easy conversation for any couple to have, especially early on in the relationship.
Before my current partner, there was a brief situationship but I’d felt too awkward to ask him if he was clean. Asking someone if they were STD-free or if they’d gotten tested somehow felt like an accusation—like I suspected them of sleeping around or engaging in risky sexual behaviour.
Not that there’s anything inherently wrong with sleeping around.
I’m not the only one who feels this way. An r/singapore thread on STD testing some three years ago turned up some comments referencing similar attitudes. One commenter said a GP appeared to be “outraged” on her behalf when he heard that her boyfriend had suggested they both get tested.
When it came to my current partner, I felt comfortable enough to broach the topic as he was open-minded and liberal from the get-go. He later told me that he’d have brought up STD testing if I hadn’t. We happened to align perfectly when it came to the topic of STD testing. Rather than getting hung up over it, we both saw it as something we should do to protect each other’s health.
And when I’d asked around the office, I found a refreshing openness when it came to the topic. A couple of other colleagues chip in with their own STD testing stories.
“I think amongst my friends, we are open to talking about STDs,” Liam tells me.
“But I think there is definitely still a stigma in general where people will think you are kind of a ‘whore’ or ‘slut’ if you have an STD.”
He chalks this up to some not being “super open about sexuality”.
As a professional, Dr Tan shares a similar perspective: “I would say there is still a huge knowledge gap in the general population when it comes to sexual health.”
He gives me examples of commonly held misconceptions about HIV and STDs, and I can’t help but cringe.
Most people believe if you have unprotected sex with someone with HIV, then there is a 100 percent chance of getting HIV. There are also people out there gargling with Listerine after oral sex to reduce their risk of infection. Others think washing your privates with Dettol will somehow keep them safe from STDs.
Sadly, there haven’t been significant improvements to this over the years.
“I think the barriers to STD screening are still the same as they were 20 years ago: A lack of knowledge. A belief that ‘it will not happen to me’. A belief that ‘I am not at risk because I do not sleep around’. Too shy to see a doctor. Turning to the internet for home cures, like apple cider vinegar for warts.”
Dr Tan candidly admits that sometimes, doctors are part of the problem. Since STDs are not a big part of medical school curriculum, some of them may not be comfortable dealing with them.
“This may add to the patient feeling more embarrassed or alienated. And maybe even getting the wrong diagnosis, treatment, or advice.”
On the plus side, he notes that more people are indeed coming to his clinic for testing over the years, although he says he cannot speak to whether this is a trend nationally. He does see some couples getting tested together, but there are “not that many”.
Peace of Mind
Beyond just being a fun date idea, it’s worth highlighting that STD testing is crucial for a number of reasons. A big one is that some STDs can have serious complications, so catching them early is important.
Take chlamydia, for example. The STD is “extremely common”, says Dr Tan.
“The scary thing about chlamydia is it can remain completely asymptomatic, especially in women. It then silently damages the fallopian tubes leading to infertility.”
Another example is HPV. If left undetected and untreated, it increases the risk of developing cervical cancer in women, and anal cancer in men and women.
Syphilis, if left untreated, can “literally make a person go mad” or destroy the aorta, which is a major artery in the body.
With all the stigma that still persists today, more education and awareness around STD testing is needed, says Dr Tan.
“A prime example is the men who have sex with men (MSM) community. The MSM community has been the target group for many sexual health outreach programs. So in my observation, members of that community are much more clued in when it comes to sexual health.”
Now that I’ve been there, done that, I can attest that the peace of mind after getting tested is worth any awkwardness you might feel.
Beyond a clean bill of health, knowing that my partner and I were on the same page when it came to our sexual health was the true highlight.
And if someone reacts negatively when you bring up STD testing, do you really want to sleep with them?






