Arguably the best episode of The Office revolves around a heart attack. Dwight Schrute, Dunder Mifflin’s best-performing salesman and worst-performing person, stages a fire drill by setting a paper bin alight the office.
Chaotic shenanigans ensue, but the theatrics end with resident curmudgeon Stanley Hudson suffering a heart attack. Cue the opening credits, but not before Michael Scott yelling that Stanley can’t die just yet because (a), he’s black and (b), Barack is president.
ADVERTISEMENT
Hilarious! But consider this awkward downer of a statistic: cardiovascular disease accounted for 32 per cent of global deaths in 2019, and remains to be one of the leading causes of deaths alongside the global pandemic that plagued 2020. Of the deaths caused by cardiovascular disease, 85 per cent were due to heart attack and stroke according to the World Health Organization.
The statistics are bleaker when you take the region into account. The prevalence of cardiovascular morbidity and its risk factors was found to be especially high in Southeast Asian countries, thanks to prevalent tobacco use, unhealthy diet patterns, physical inactivity and harmful alcohol consumption.
So while we might not have Dwight Schrutes in our workplaces (I hope), the risk of collapsing from a heart attack due to work burnout remains very much real, both at home and at the office, even as we slowly return to normalcy.
Cardiology Calibre
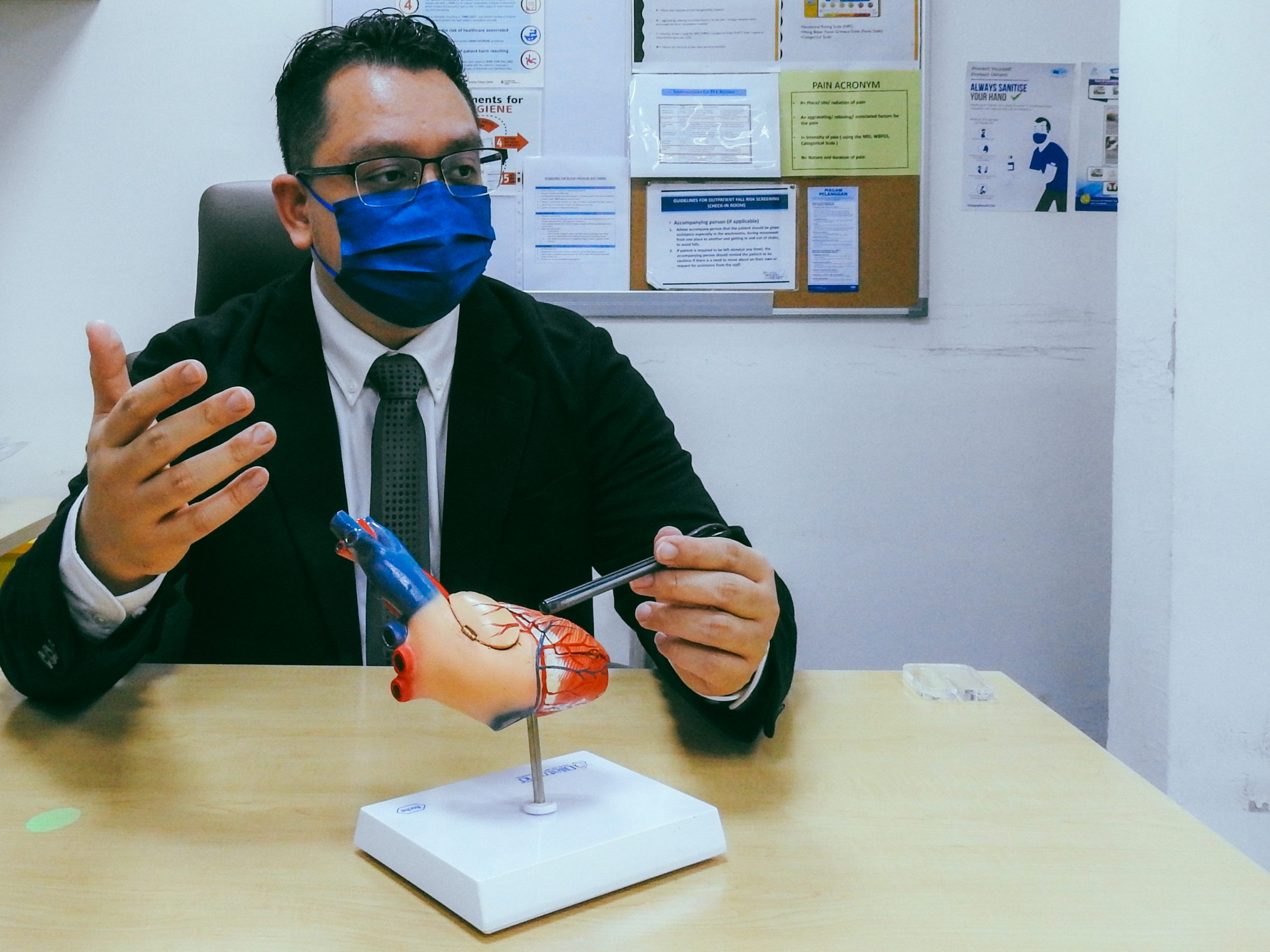
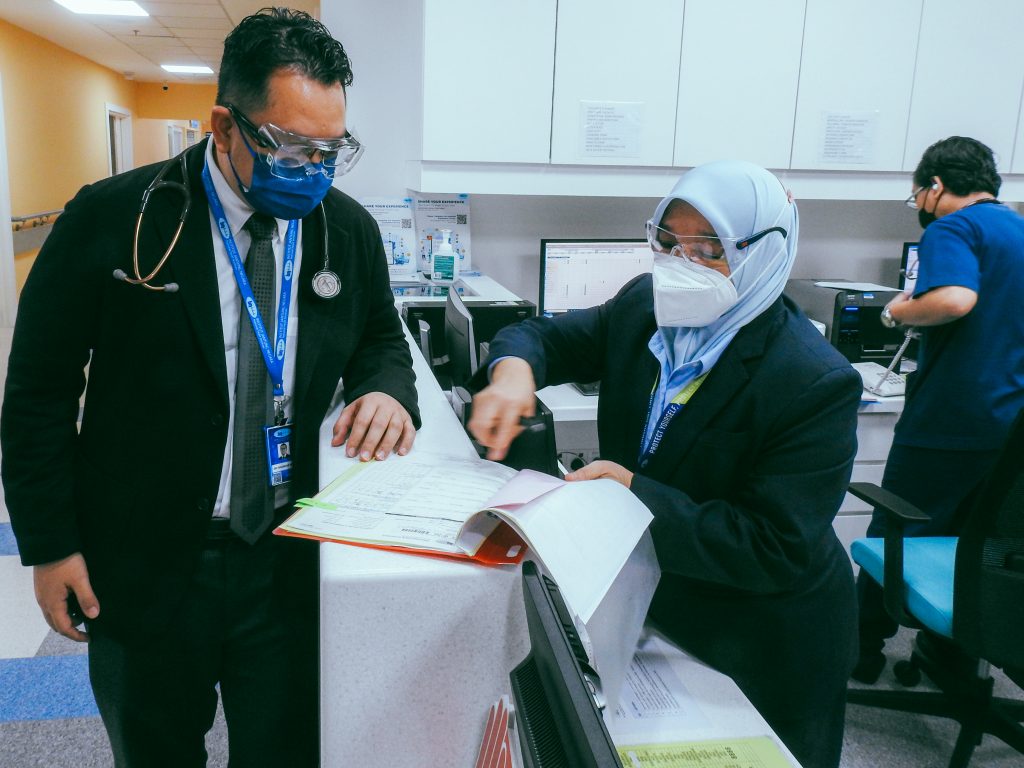
Medically speaking, how do we live long and prosper? Dr Iskandar Mirza Amran, a Clinical Fellow in Cardiology & Internal Medicine Physician in Malaysia, offers some wisdom.
The 35-year-old doctor is part of a diverse team of experienced medical specialists supporting Malaysia’s reputation as the Cardiology Hub of Asia. Supplemented by the state-of-the-art devices, equipment, and technology in hospitals across the country, Malaysian institutions have earned the trust of patients worldwide to deliver the utmost excellence in everything concerning heart health.
Dr Iskandar got his start in internal medicine more than a decade ago, with a specialty in cardiology from The Royal College of Surgeons in Ireland. Following a medical stint in Negeri Sembilan, the doctor now practices in Kuala Lumpur, where his daily routine consists of cardiac evaluations and surgical interventions, unblocking coronary arteries, repairing heart valves — pretty much anything that involves restoring the function of the body’s circulatory system.
Of course, the first thing I asked the doctor was how he has been holding up with the ongoing Covid-19 situation in Malaysia. The man didn’t hesitate to offer that he shed 13 kilograms over the last three months, no doubt due to the exponential increase in workload and patients that need treatment.
“In one day, we can take on up to 20 to 30 cases of angiograms (diagnostic tests that use x-rays to take pictures of blood vessels) and discharged cases can go up to 30 to 50 per day,” Dr Iskandar openly shares.
“But so far I’m holding on very well. I’m happy with the weight loss! I didn’t use to look like this — I was a bit chubbier before,” he laughs.
As the world prepares to live with Covid-19 as an endemic, Dr Iskandar offers ways of living longer today when our focus on holistic health is crucial more than ever — be it global viruses or heart issues.
I want to ask about Malaysia’s cardiology institutions and the country’s positioning as the Cardiology Hub of Asia. Why do you think people flock to Malaysia to get cardiac treatment?
ADVERTISEMENT
Malaysia is home to 58 cardiothoracic surgery specialists, over 200 cardiologists and more than 40 centres with facilities certified for cardiac excellence. The equipment we have on hand is state-of-the-art, giving us the capability to treat a wide range of cases of varying complexities.
Our globally-accredited hospitals have welcomed a large number of international patients from over 10 countries, with the youngest patient treated being as young as 6-months-old. Most of the patients I’ve personally received are from Indonesia, while others come from Singapore and Vietnam.
Patients usually seek a second opinion regarding their heart problems. When it comes to invasive procedures like open-heart surgeries, some patients don’t like it, they don’t want it. So they are willing to seek other kinds of procedures where medical consultants can perform less invasive techniques like drug treatments.
But when they do need intensive treatments, they fully entrust us to deliver.
What are some of the common tests that patients seeking cardiac treatment undergo in Malaysia?
What we do first is ask questions to check if the patient holds any identifiable symptoms of heart problems, like shortness of breath, or if they easily get tired. And if they do, we proceed with further investigations through specific tests.
One of the first things we do is run an electrocardiogram (ECG) to record the electrical signals in your heart. It’s a painless procedure that involves sticking electrodes to your chest. From here, we can assess the heart’s rhythm, whether it’s beating normally or abnormally.
Then there’s echocardiography, an ultrasound scan of the heart. And from here we can see the structure of the heart — whether it is pumping normally, whether the valves are opening well.
There’s also a blood test we run called a Brain Natriuretic Peptide (BNP) test, which measures levels of a protein called BNP. The heart produces two main types of substances: BNP and N-terminal pro b-type natriuretic peptide (NT-proBNP) — these are released in large amounts when the heart senses that it needs to pump harder.
So, if your BNP or NT-proBNP levels are higher than normal, it probably means you have heart failure. High levels of these substances in your bloodstream can mean your heart isn’t pumping as much blood as your body needs. Immediate treatment can be offered. For example, there’s the Parachute Ventricular Partitioning Device for heart failure patients — Malaysian hospitals were the first in Asia to use it in 2013.
For young patients with a risk of cardiovascular disease, we offer exercise stress tests: we put electrodes on their chest and ask them to carry out some exercises. For those who can’t do physical activities, we give them medication that increases their heart rates. Those with partially blocked blood vessels will have abnormal heart rates because blood is not being pumped properly when a person is stressed. We can analyse which part of the blood vessel is affected and proceed with an angiogram.

Speaking of young people, can someone actually be too young or too fit to worry about heart disease?
When you say that, I’m thinking of sudden cardiac death among young athletes. This usually involves abnormally-large heart muscles.
The most common disorder is called hypertrophic obstructive cardiomyopathy (HOCM) — this involves heart muscles that are abnormally thick, making it harder for the heart to pump blood. It’s very common among those who die before reaching 40. So, it’s very important to conduct a post-mortem if we suspect that they have HOCM.
This is a congenital disease that can be inherited and often goes undiagnosed because people can live normal lives without being aware of it. They might not know they have it in the first place because it’s a progressive disease that might not show symptoms until they reach 30 years of age and above. If we detect HOCM following a post-mortem of the deceased, we can screen their family members before the disease affects them.
What we can do for those diagnosed with HOCM is a surgical resection of the heart muscle. Or we can install a pacemaker to regulate the heartbeat when the heart rhythm becomes erratic, preventing them from sudden death.
I’d normally associate pacemakers with older people.
It’s true, most of the patients we treat are older. Getting pacemakers fitted is a common procedure for those aged 70 and above.
However, we do have younger ones too. There are instances where patients among the younger age groups may require one as part of their treatment and avoid suffering complications due to strenuous activities or moments of heightened anxiety.
Here in Malaysia, we’ve had numerous impressive successes in the realm of pacemakers. We are the first in Asia Pacific to conduct in-man trials for the world’s smallest pacemaker: the Medtronic Micra Transcatheter Pacing System (TPS). It detects when a patient’s heartbeat slows down and deliver a small shock to normalise the rhythm.
The National Heart Institute (Institut Jantung Negara) were the first hospital outside of the USA to implant a Micra AV pacemaker. It’s an advanced technology that we call a leadless pacemaker. It’s the size of a small bullet that is implanted on the surface of the inner heart, with a battery that lasts for years. That’s the best technology we have in Malaysia.
The traditional ones typically consist of a big lithium battery on the upper part of the chest with a lead going through the heart.
How easy is it for us to get heart diseases?
I don’t know about Singapore… but in Malaysia, we have plenty of mouth-watering food from various ethnicities enjoyed by people from all around the world. A diet consisting of food with high cholesterol and high sugar is one of the main factors that cause cardiovascular diseases.
Most people tend not to go for medical screenings. By right, we should go for one at least once a year so that we keep track of our cholesterol levels, blood pressure, or find out if we have any underlying diseases such as diabetes. These three issues — plus obesity — can lead to metabolic syndromes that further increase the risk of heart attacks.
To minimise the risk of heart diseases, it is encouraged to consume less sugar and salt. Some foods such as satay, rendang, and nasi lemak, are high in cholesterol and fat due to the ingredients used, like santan (coconut milk). While we can enjoy such sumptuous food, we need to regularly educate people to eat moderately to prevent cardiovascular problems.
Some drastic lifestyle choices need to be made, I suppose!
It’s also very important for us to exercise regularly. You don’t even need strenuous exercises like running or swimming. Brisk walking 45 minutes a day is enough to make you healthier.
The next thing is, of course, maintaining a healthy diet. If you ask the American College of Cardiology or the European Society of Cardiology, they will recommend going for the Mediterranean diet as it consists mostly of fish, fruits and vegetables.
For those with high blood pressure, high cholesterol and diabetes, I recommend doing both. Reducing about 10 per cent of your body weight will improve your cardiovascular health.

What are your thoughts on the trend of alternative meats these days?
It’s great that people are moving towards plant-based diets and reducing their meat intake. It has been proven that if you adopt a vegetarian diet, it markedly reduces the risk for cancer, stroke and cardiovascular diseases.
The only problem? Whether our people can adopt the diet or not. If they can’t, what I would recommend most people to do is reduce their rice intake. High intake of refined carbs is linked to obesity and chronic disease.
But it’s not just about diets, it’s also about lifestyle choices. Take smoking, for example. The youngest patient I had who suffered a heart attack was 18-years-old because of chronic smoking. I have seen kids who started smoking at the age of 10 or 11. So by the time they turn 18, it’s not surprising that they get heart attacks. It’s quite sad — what we need to do is to continuously educate, promote healthy lifestyles and its benefits.
Let’s talk about smoking then. What are your thoughts on e-cigarettes and vaping as the supposedly healthier alternative?
It’s not. Last year, the European Society of Cardiology released a study revealing that e-cigarettes deliver high amounts of nicotine that stiffens blood vessels and arteries.
When blood vessels become stiff, it becomes easily injured, and when the inner layer of the blood vessel is injured, the first substance that stops the injury is fat. With repeated stress, more and more cholesterol will actually deposit in the same spot. And this will cause a blockage of the blood vessels. So, yes, vaping can cause heart attacks.
As vaping is illegal in most countries, most of the younger patients who come in to get checked won’t disclose that they vape. It’s hard to study the long term effects of vaping on heart diseases if they don’t admit to it. So until then, we’ll keep referring to the studies carried out in Europe.

This might be a weird question… but how would you explain the chest pains you feel when you get heartbreaks?
An interesting question! It’s relatable because everyone gets anxious when they get heartbroken. Your heart sees the need to pump faster, increasing the adrenaline inside your body. Similar to how one may be chased by something; your brain tells your adrenal glands to secrete more adrenaline so that you can run faster.
There’s a term called broken heart syndrome, or takotsubo cardiomyopathy. When there is a persistently high adrenaline rush within the body, it will cause the blood vessel of the heart to get constricted. And when less blood goes to the muscle, the cells actually die off one by one, because there’s less nutrition and oxygen feeding the cardiac muscle. One will experience shortness of breath, chest pains, and heart failure can occur.
But it can be treated. We can give medications like aspirin to thin the blood so there’s less burden on the heart to pump. Beta-blocker tablets can help slow down the heart rate. Some patients will see improvement while some others don’t. Regardless, broken heart syndrome is a serious medical condition that is often not diagnosed properly.
Damn. Maybe let’s talk about something that’s even more relevant these days — the relationship between Covid-19 and cardiovascular issues. How does each affect one another?
We have a lot of studies that show that those with cardiovascular risk factors — like high blood pressure, diabetes, obesity — tend to have severe Covid-19 infections compared to those who don’t. If we compare one patient with high blood pressure and another one without, you can see that the patient can have a Category 3 or higher Covid-19 infection compared to those without high blood pressure.
Covid-19 worsens any prevailing condition. For those with high blood pressure, they have this receptor called the ACE 2 receptor. When we want to treat a patient with high blood pressure, we give ACE inhibitors because they will bind with the receptor and reduce blood pressure.
That’s why we’ve been facing a lot of referrals because there are quite a number of Covid-19 patients who get heart attacks. It’s bad because Covid-19 can increase the risk of thromboembolism, where blood clots break loose and can go anywhere in the body.
If blood clots hit the brain, it causes a stroke. If they go to the heart, it causes heart attacks. If they hit the kidney, the kidney fails. All these, on top of severe lung inflammation due to Covid-19, result in less oxygen going to the heart. This leads to eventual death.
Medically speaking, how can I live longer?
To live life to the fullest, you have to first take good care of yourself and never compromise on your health. Eat a balanced diet, exercise regularly, go for frequent health checkups and never miss your medications if you’re already on them. By having a healthy lifestyle, the possibility of getting heart disease reduces markedly. The quality of life increases.