All images provided by the profile.
In the early days of my life as an paediatric hematologist and oncologist in Malaysia dealing with childhood cancer, life was a lot tougher than it is now. I’m talking about the 90s, back when technology wasn’t as advanced and there was a huge shortage in manpower in the healthcare industry.
Paediatric oncology, in particular, wasn’t a very popular specialty. As you can imagine, it’s a very demanding job — you’re dealing with kids with cancer after all. It can take a very distinct mental and emotional toll on you.

As part of my four-year training as a paediatrician back then, we were required to undergo postings in the various subspecialties. The field was shorthanded, but I had a keen interest in dealing with young ones since those days and chose to pursue it.
I joined the unit on a full-time basis in 1993. Since then, many kids have come and gone — there are happy endings and not-so-happy endings. But that’s only part of the job.
Journeying With Patients
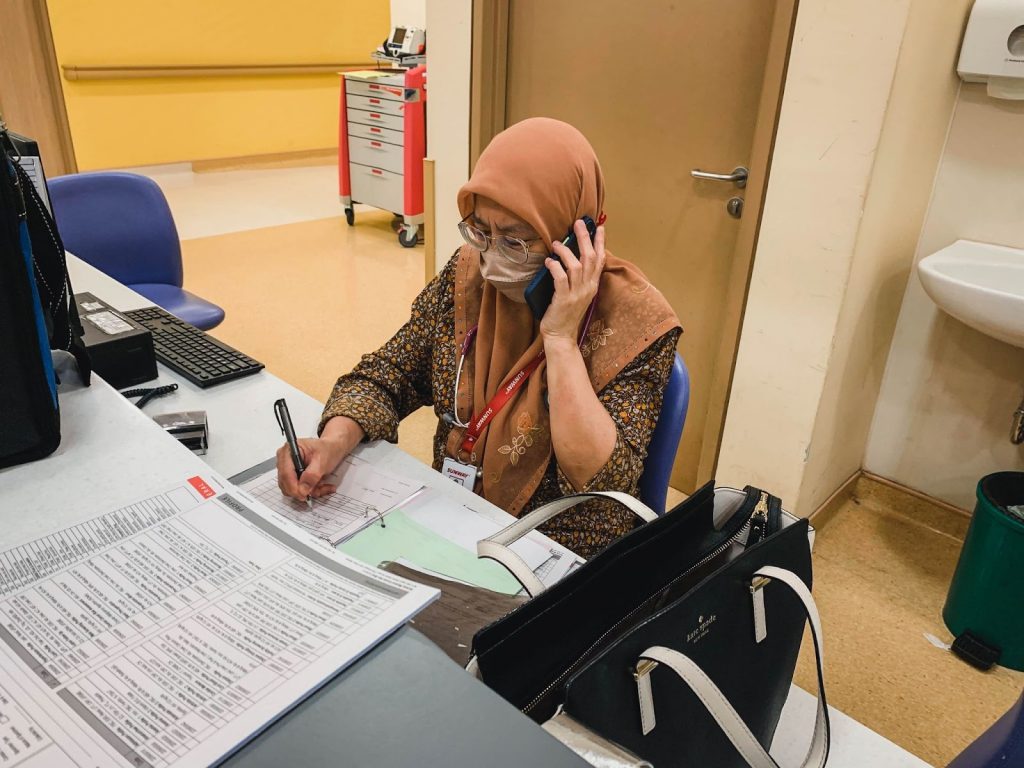
When we say work ends at 5pm, that’s not usually the case. On any given day, work hours can stretch to 10pm, even way past midnight. Every so often, a child develops a new problem or a new case decides to land on our doorstep. In any case, we would need to be ready to address them.
In the past, paediatric oncology units in Malaysia were concentrated in the Klang Valley. Patients would arrive as early as 4am as they would have taken the night bus and travelled a far distance from different states — Johor, Penang, and the East Coast. They need to be seen and sorted as early as possible so that they can return home at a decent time.
People don’t realise this, but doctors who care for children, like myself, often suffer with their patients. You journey along with them through these ups and downs, yet try to be detached at the same time. But we are only human, and it can be hard to remain completely detached because you’re so deeply involved in their care.
Just when you think they’re recovering, sometimes their cancers may very well choose to relapse — in the primary site, metastatic or both.

Why am I still doing this? I’ve questioned myself many times and even thought about quitting at one point. It’s normal to feel mentally burnt out after a period of time, right? You can’t just pack up and leave. Technically, you can. But that isn’t right. What I do is take a step back and take a break sometimes.
I can’t deny that the job’s meaningful despite all that. We follow these patients till adulthood. Looking at the long-term survivors, I am very proud of them — of how much they have come through and what they have made of themselves.
Knowing that you have had the opportunity to be part of their lives and help contribute to their care keeps me going. I guess that’s why I’m still here after all these years.
Healthcare has advanced tremendously since my years as a junior doctor in training. We’ve gotten a lot more specialists onboard; manpower has improved and we’re in a much better place than before.
Kids With Cancer
People tend to forget that kids get cancer, but even children below 1-year-old can be diagnosed with it. Yes, I’m talking about babies who are only months old. I’ve seen little babies battling cancer, even those who can barely walk yet.
The most common form of cancer amongst children is Leukemia — it makes up for one-third of all childhood cancers that we see. The problem with childhood cancer is that the symptoms and signs may be very subtle.
They often mimic common childhood illnesses like infections and fevers, but it’s a worrying sign if they don’t recover after some time, or if symptoms keep recurring even after trips to the regular clinic.

If a child develops swelling in the arm, or if they run and constantly fall… all these can be attributed as a result of trauma. As time goes by, soft tissue injuries should resolve. When they persist or grow in size, it’s a sign to examine further.
Because these signs are so subtle, there’s always a degree of delay — it’s not surprising that by the time patients come in, the disease could be at an advanced stage.
It’s also interesting how grown-ups often express how bad they feel when looking at kids who’ve been diagnosed with this terrible disease. Many people don’t know this, but the outcome for children is actually much better than for adults.
Kids tend to respond better to treatments as they don’t usually have other prevailing health problems such as hypertension, diabetes; things that adults might have. Leukemia used to be a tricky situation if you’re looking at the 1960s when technology was less advanced, but we’ve come to a stage where the cure rates can be as high as 90 per cent.

For the most part, we see most of these cases as potentially curable. The real challenge is that survivors may suffer from effects caused by the very treatments that helped save their life. Many of these effects, such as liver, heart or kidney problems may pop up later in life.
Our goal then is not just to cure. The goal is to cure with minimum costs in terms of late-life effects. We have to remember that anyone who has had cancer has the risk of getting another later on. Treatment is still ever-evolving — what we hope is that these children grow up with as little risk as possible.
Sure enough, I’ve had plenty of patients who’ve been with me since they were little kids. I’ve watched them grow into functional adults with a whole life ahead of them. Some even get married and return for regular health checks with their partners and offspring.
I joined my current centre in 2019 and have been working here since. That was the pre-pandemic era, so patients were coming to Malaysia from all over the region — Cambodia, Indonesia. Things were quiet during the lockdowns but now that the situation has improved, we are starting to see the return of international patients again.
Despite the distance, many of them choose to fly all the way for a variety of reasons — for one, they might not get the same quality service for Pediatric Oncology that they’re looking for in their country, or they might be hard to reach, whereas Malaysia Healthcare is a reliable hub, with many private healthcare facilities.
We offer treatments that are relatively affordable too if you’re comparing medical costs to other modern cities like Singapore. Regardless, they travel all the way, and they entrust us to deliver.
Things Left Unsaid
I’ve once had a female patient; she was slightly older — 15 to be exact. She was paralysed from the waist down because of a tumour that had gone into her spinal cord. We gave her multiple treatments and she actually managed to make a complete recovery after some time.
She was a very resilient person; always making plans for her education and career. She continued to fight on even when her neuroblastoma (a disease in which malignant cancer cells form in nerve tissues) kept recurring.
Even when she became an adult, we still saw her as our child. She will always be.

Even with all the odds stacked against her, she did go on to achieve all that normal life stuff up to the very end. In fact, she led a full life with good friends and supportive employers till 30 when she lost the fight.
I’ve seen her grow from 15 to 30, and I do think about her every now and then, as I struggle to contain my personal emotions. It is said that we can learn a lot from kids, and that’s especially true from seeing the positivity and strength displayed by patients like her.
We have programmes such as the Celebration of Life, where patients who were deemed to have been cured return for a get-together; sort of like a huge support group.
It’s saying to current patients: “Look, these are people who were treated back in the 90s when treatments were not as advanced. It sucks, but you can conquer it too.”
Support makes a huge difference for many of these patients who missed a chunk of their childhood. They need as much hope as they can get. As do doctors. Looking at all these past patients who’ve moved on with their lives as regular people, we get to see the impact of our work. It keeps us motivated.

We often tell parents to let their children go back to the norm — school life, making friends; whatever it is to make them feel like everyone else. They need that as much as possible. The last thing you want is to overprotect and resist to a point where it’s too late. There are some children who never had a chance to experience life at all.
There’s no formulaic way to convey the truth to patients and family, but I’ve learned better than to say things like “everything is going to be ok”.
Younger kids, especially those under five, are probably not aware of what’s going on. But the older kids who already understand the concept of death have a lot of questions and concerns. This needs to be addressed as best as possible.
It’s never a good idea to hide children from the truth, worse still to “lie”. In this social media-driven era, they can learn all that we don’t tell them online — and it may not always be accurate. We encourage parents to be as honest as possible, especially on the different treatments and procedures that they have to go through.
Not having these conversations early enough may lead to more confusion and pain down the road. If they don’t understand what they need to go through and why, there will be resistance; even refusal to come to the hospital.
It could lead to a mess of regrets over things left unsaid, or potential treatment options that should have been pursued earlier.
The Unspoken Qualities of a Doctor
Over the years, I’ve worked with families that come from different backgrounds, including those from lower-income groups. One parent could be at the centre with the kid while the other is working. Siblings also have needs — not having either parent around is tough for them too.
Understandably, they are troubled and upset at the situation. In a way, doctors are like therapists. Sometimes, what these people want is just a listening ear.
There’s a whole set of skills we need apart from medical knowledge. Being a doctor has taught me to be truly empathetic towards people’s hopes, dreams, and fears. Just being there takes a lot, but it’s the least we can do when they are going through a tough time.
Above all, I think there is a need to create higher awareness about childhood cancer. Some people think chemotherapy is bad; that it will harm their kids. Or even worse, they might be in complete denial if doctors tell them about their kids’ diagnosis.
Increasingly though, more people are coming forward as time moves on and that’s a good thing. Again, it goes back to awareness.
Each small joy is worth celebrating. Each kid that comes by is a feat of strength reminding me of my reasons for choosing this profession and the need for us to keep moving forward.
When you deal with patients with chronic illness, burnout is normal. You’ll reach a point and say to yourself: ‘Enough is enough.’ Seeing these children fight on to make something out of their lives, and knowing you can help to make a difference is what keeps most of us going.







